Last partial update: July 2016 - Please read disclaimer before proceeding
(Back to top)
The lifecycle of acne
Acne is a very common condition that particularly affects adolescents, with about 95% of this group being affected to some extent. It is inherited to a significant degree and brought on by the increased production of male hormones (androgens) that normally occurs in both males and females during puberty. Females go through puberty before males and thus present earlier; usually in their early teenage years. Males present later and generally with more severe disease.
It usually starts on the forehead and chin and then later spreads to the cheeks. In worse cases it involves ears, neck, scalp, back and chest. The condition tends to gradually worsen through puberty and is usually reaches its peak in 14 to 17 year old females and 16 to 19 year old males. After the age of 25 years, about 12% of females and 3% of males are still significantly affected. (Acne is common in post‐adolescent women with polycystic ovarian syndrome.)
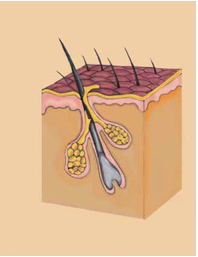
Acne originates in the pilosebaceous glands of the skin. Sebaceous glands are glands that produce sebum, an oily substance that coats the skin, helping to 'condition' it. These glands usually open into a hair follicle and the sebum they secrete exits via the hole around the hair. Thus, these glands are also responsible for the oily coating on hair. Together, the hair follicle and its associated sebaceous gland are called a pilosebaceous gland. (pilo ‐ hair)
While acne is not a preventable illness, it is very treatable. It can cause considerable suffering and can contribute to anxiety and depression in some adolescents. For this reason it is included in this web site.
Dermis (Area under pink epidermis layer)
Keratinocytes are the pink cells lining the gland and hair follicle. (They also make up most of the epidermis.)
|
(Back to top)
What causes acne?
The following events in the skin's pilosebaceous gland cause the development of acne.
1. Excess sebum production: An increase in the level of male hormones (androgens) causes excess production of the sebaceous gland's oily secretion (called sebum). It does this by increasing the size of the glands and there is considerable variation in the effect of male hormones on individual glands. This is why some areas of the skin are affected more than others.
2. Excessive turnover of keratinocytes (gland lining cells): The same hormones cause an increase in the turnover of the skin cells that line the inner wall of the gland (called keratinocytes). This leads to two problems. Firstly, it thickens of the gland wall and this thickening acts to obstruct the gland outlet. Secondly, it results in more dead keratinocytes (lining skin cells) being sequestered into the gland. These dead cells also tend to be ‘stickier’.
3. Excess cells and sebum cause blocked glands: white heads and black heads. This increased amount of sebum and dead sticky skin cells lead to the formation of small collections of dead cells called 'micro‐comedomes' which act as plugs that block the exit duct of the gland. The blocked gland continues to produce oil but it cannot escape and the gland swells slightly. These are seen as small slightly raised lumps on the skin with or without some white‐ looking material below. There are often termed white‐heads and there are usually lots of them. Where the top of the plug or comedome is exposed to the air, it turns a dark colour; a lesion commonly called a 'black‐head'.
4. Bacteria grow in blocked glands: The conditions in these blocked glands encourage the growth of a bacterial species commonly present on the skin called Propionibacterium acnes. This bacteria is not harmful but can cause the surrounding gland to become inflamed (red and more swollen).
5. Swollen glands can rupture, leading to scarring: All this can lead to significant swelling and finally rupture of the wall of the sebaceous gland and the contents then spread into the surrounding skin tissue (called the dermis). This results in more inflammation and the occurrence of cysts, which are felt as painful lumps under the skin. These can get fairly large. The lesions eventually heal but in doing so can leave scaring. In dark skinned people this scarring can also be associated with pigmentation changes.
Acne and diet
There has been much debate about whether diet influences acne. It was long held that diet was a significant factor. Some years ago this view was overturned and until recently it was believed that diet was not significant. However, a recent study has shown that this may not be the case. It showed significant improvement after three months in 50% of those affected who consumed a high protein/ low GI (glycaemic index) diet rather than a typical teenage diet high in processed foods. This study was small, looking at only 50 adolescent boys, and further evidence needs to be gathered
supporting these findings. However, the diet is a relatively healthy one and certainly is likely to be healthier than a normal teenager's diet. It will certainly do no harm for teenagers to try it out. A teenage anti‐acne diet booklet based on the diet in this study has been published by the Australian Women's Weekly together with Meat and Livestock Australia; the organization that funded the study. It promotes a higher‐protein, low GI diet and has been supported by the President of the Australian College of Dermatologists. (The diet is higher in protein than the diet generally recommended for the adult population.) This booklet can be downloaded from the following site. http://www.themainmeal.com.au/Red+meat+and+nutrition/Teenage+anti‐ acne+diet/Teenage+anti+acne+diet.htm
Excessive picking of lesions
This is unfortunately quite common in teenagers and if it persists it can turn mild acne, that results in little long‐term scarring, into a life‐long disfiguring condition that causes life‐long facial disfigurement. Picking lesions does not help.
Excessive facial washing
Facial washing can not reach deep enough to remove comedomes or the bacteria that lie in the blocked ducts below them and thus excessive washing is of no benefit. All it does is make inflamed lesions worse, especially if the washing is done aggressively.
Cosmetics and sunscreens
Most are formulated so that they will not make acne worse. However, those containing oil can cause a problem and cosmetics should not be caked on.
Medications
Some drugs can worsen acne, including anti‐epileptics, steroids, cyclosporin and lithium. Most forms of the oral contraceptive pill improve acne but a few can make it worse. It is usually the progestin that is responsible.
The use of illegal anabolic steroids to promote muscle growth in young male athletes can make acne worse.
Other conditions
Some medical conditions are associated with acne. The most common one is polycystic ovarian syndrome, which occurs in up to 10% of women. This is usually also associated with being overweight and irregular menstrual periods. If this combination of symptoms is present, polycystic disease is worth considering. This diagnosis, which is mostly based on symptoms, has other health implications. Other hormonal problems that cause an increase in androgens can cause acne as well and should be suspected if acne is more severe.
(Back to top)
How bad is my acne?
Acne in adolescents is often a very emotive condition and severity a relative thing. Below is a general guide for classifying acne severity that includes the treatments usually prescribed.
Severity |
Features |
Distribution |
Usual treatment |
Mild acne |
Blackheads (Comedomes reach the skin surface. The black colour is not dirt and is probably due to oil in the comedome reacting with the air.) White heads (Comedomes that stay below the skin surface) |
Involves only part of face, commonly forehead and chin. |
Good skin care / healthy diet Topical medications, usually retinoids plus anti-bacterials in warranted. |
Moderate acne |
Lesions are infected by bacteria causing: Papules - Raised red lumps are present Pustules - Raised red lumps with yellow or white centres. |
More generalised on face and on back and chest. |
Good skin care / healthy diet Topical treatments Oral antibiotics Hormonal treatment in females |
Severe acne |
Bacterial infection worsens Nodules and cysts develop, appearing as solid painful lumps under the skin |
Covers large areas of body and face. |
Treatments for moderate acne plus option of adding oral retinoids. |
Treatment of acne - Skin care and diet
1. Cleansing
This should be done morning and night using a cleanser for sensitive skins, not one for acne. Cleansing should include removing any make up.
Cleansers should not contain additives such as herbs, fragrances, vitamins, fruity acids etc.
Face washing directly under the shower head should be avoided as it may cause excessive dryness and redness.
DO NOT use exfoliants, Buf-Pufs, alcohol or acne wipes, toners, scrubs, granules, masks, peels, steams or have facials.
2. Moisturising
If skin becomes excessively dry with treatment, an appropriate moisturiser can be used twice or more per day. This will not exacerbate acne. Do it straight after face washing, before acne treatments or sunscreens are applied.
The moisturiser should not contain oils and should be formulated to not cause pore blockages.
Again it should not contain additives.
3. Sun screens
During acne treatment skin is often more sensitive to the sun and thus sun screens should be used. They should be oil-free and 15+ or higher. Some may aggravate acne. If this occurs try another one.
4. Diet
As stated above, there may be some acne-reduction benefit in adopting a higher-protein, low GI diet and certainly the diet recommended by leading dietitians and the Australian College of Dermatologists is likely to be healthier than that being consumed by many adolescents.
The Teenage Anti-acne Diet booklet
Treatment of acne - Medication
General comments
In general, acne is best treated by attacking the problem in several different ways. The methods of treatment available include:
- Treatments that return gland lining cell turnover (and thus gland wall thickness) to normal
- Topical retinoids
- Azelaic acid
- Salicylic acid and glycolic acid
- Treatments to reduce bacterial numbers in the glands
- Topical antibiotics
- Topical bactericidal drugs
- Oral antibiotics
- Treatments to reduce androgen hormone action on the skin glands
- The combined oral contraceptive pill ('the pill')
- Oral spironolactone
- Treatments to reduce sebum production in the gland
- Oral retinoids
Most treatments take two to three months to work. The promises of quick-fix therapies often promoted in the media are very misleading and create unrealistic expectations of prescribed treatments and this unfortunately leads to teenagers prematurely giving up on treatments. It is important to give treatments adequate time to work.
Sometimes there is actually a flare up in acne about four to six weeks after treatment starts. This can be due to either bacterial death which actually causes more inflammation, or it can be due to the unblocking of blocked ducts. Once these temporary events subside, the flare up settles and an overall improvement will occur, usually in a couple of months.
Most acne treatments only act to relieve symptoms while they are being used. They do not cure the disease. Thus they need to be used for extended periods, often several years, until the disease runs it natural course and subsides. The exception is oral isotretinoin which causes long term improvement with a single course in most people.
Topical treatments in general
Topical treatments work well and often are all that is required in mild to moderate cases. As stated above, creams can work either by returning cell turnover in the glands to normal or by killing bacteria. It is usually best to use combinations of treatments. (Such a combination might include a topical antibiotic, a topical retinoid and an application of benzoyl peroxide.)
Most acne creams act to dry out the skin which in turn unblocks the ducts. This drying out process can also cause some irritation and redness. This means that only a gentle cleanser should be used on the skin and toners, scrubs, masks and steams should be avoided.
Initial treatment is generally for 12 weeks but most teenagers require long term maintenance therapy. Topical retinoids are a good choice and are preferred to topical antibiotics, the long term use of which is likely to promote the formation of bacterial antibiotic resistance.
As most creams cause irritation it is important to avoid contact with sensitive areas such as lips, nostrils, and especially around (and in) eyes.
A. Treatments that reduce excessive cell production that blocks ducts
Topical retinoids
These medications normalise the turnover of the lining cells (keratinocytes) in the gland which returns gland wall thickness to normal. This reduces gland blockage and thus future comedom formation and future inflammation. It also helps penetration of topical antibiotics.
Initially this process results in extra lining cells being sequestered into the gland and at about 3 weeks after treatment commences, this causes increased pressure in the glands and the expulsion of comedoms that are blocking the gland. This process causes a mild exacerbation of acne. This soon settles and the maximum beneficial effect occurs two months later.
Topical retinoids produce skin dryness or irritation (or dermatitis). This is minimised by introducing them gradually, building up over a few weeks until normal application an be tolerated. This is usually achieved by washing it off sooner than normally recommended each night and most manufacturers provide recommendations about how to go about gradually increasing the application time. An additional option is to use it every second night initially. Appropriate skin care is important, especially the use of moisturisers. Sun sensitivity is also a common problem. It can be overcome by applying creams at night and by the daily application of sun screens. The skin should be cleaned and dried well before the cream is applied.
Care needs to taken with application so that the cream or gel does not contact more sensitive parts of the body such as lips, around nostrils and especially close to and in eyes. Also any areas of sunburn should be avoided.
Topical retinoids should not be taken if there is any likelihood of pregnancy as they can cause foetal abnormalities.
Topical retinoids are a good first-line treatment for mild to moderate acne with effects generally taking about 12weeks to occur. Available medications include:
- Adapalene (Differin) - Causes less inflammation / irritation as it has an anti-inflammatory effect as well
- Azarotene (Zorac)
- Isotretinoin (Isotrex)- Not as effective as tretinoin
- Tretinoin or all trans Retinoic acid or tretinoin (Retin A, Stieva A, Retrieve) - Probably the most potent (but also has more irritant effects)
Azelaic acid
This naturally occurring acid acts by normalising gland cell (dead keratinocyte) content and also helps kill bacteria. Good for mild acne. It is available in a 15% gel (Finaceal
Salicylic acid and glycolic acid:
These are the compounds present in most over-the-counter acne preparations. They cause skin desquamation (remove outer layers of skin) and this helps remove the comedoms that block glands. They do not work as well as topical retinoids.
B. Treatments that reduce bacterial numbers
Treatments that act by killing bacteria are either topical or oral. One problem that can occur with all oral and topical antibiotics is resistance of the bacteria to the antibiotic. This is especially common oral erythromycin and it is not often used because of this. Luckily bacteria do not develop resistance to topical benzoyl peroxide and for this reason antibiotic treatment is almost always combined with this medication. Most antibiotics also act by helping reduce inflammation.
Topical antibiotics
Topical antibiotics are effective but act more slowly than oral antibiotics. The antibiotics commonly used are clindamycin and erythromycin. They should not be used as single therapy as this causes resistant bacteria to form. (They can be used with oral antibiotics or topical benzoyl peroxide.) Side effects are mild, usually just slight irritation.
Topical benzoyl peroxide
Benzoyl peroxide inactivates the acne-causing bacteria. As stated above, unlike oral antibiotics used in acne treament, acne-worsening bacteria do not develop resistance to benzoyl peroxide. Oral antibiotics should therefore be used in conjunction with benzoyl peroxide to prevent resistant bacteria forming.
Benzoyl peroxide comes alone in several preparations and also in conjunction with a topical antibiotic (clindamycin) in a gel ('Duac gel')
Side effects include dry red skin and bleaching of towels / clothes (common). Occasionally allergic rashes occur. It also inactivates topical retinoids.
Oral antibiotics
These are a safe and effective form of treatment for moderate to severe acne. They work by killing bacteria and reducing inflammation. Erythromycin and the tetracyclines are the commonly used antibiotics. All oral antibiotics should be used with topical benzoyl peroxide to reduce the risk of resistance occurring.
Oral antibiotics work better when used with topical retinoids.
Tetracyclines: The two commonly used are minomycin and doxycycline and there is little difference in effectiveness. Generally they are well tolerated. Common side effects include vaginal candidiasis (thrush), gastrointestinal upset and skin rashes. Sun-sensitive skin reactions are more common with doxycycline, while minomycin can produce a vertigo-like dizziness and more rare serious effects including liver complications and lupus-erythematous-like reactions.
Erythromycin: Commonly causes gastrointestinal upset. Bacterial resistance rapidly occurs to erythromycin and thus it is usually only used where tetracyclines are contraindicated; mostly in children, pregnant women and those who do not tolerate tetracyclines.
C. Treatments that reduce excess androgen production
Combined oral contraceptive pill (COCP) - 'The pill'
As a major cause of acne is an increase in the male hormones (androgens), it should not be surprising to learn that hormonal treatments that reduce the effect of androgens work well to reduce acne. Most combined oral contraceptive pills (those containing both an oestrogen and a progestin) are effective in reducing acne by reducing testosterone effects. The component responsible for the androgen effect is the progestin and while some progestins can actually increase androgen effects (and thus acne) most have a slight anti-androgen effect.
This effect reduces acne by reducing sebum production and this helps both non-inflammatory (mild) and inflammatory (more severe) lesions. Generally it takes three to six pill cycles for an effect on acne to occur.
Some newer COCPs contain progestins that have a more prominent anti-androgen (and thus better anti-acne) effect. These include COCPs containing the progestins cyprotene acetate (Dianne-35 ED, Brenda-35 ED, Estelle-35 ED, Juliet-35ED), dienogest (Valette) and drospirenone (Yasmin). Pills containing cyprotene are the most effective but they also tend to have increased side effects, such as slight weight gain, breast tenderness and mood disturbances. If such side effects are a problem, then one of the other COCPs mentioned above should perhaps be tried.
The COCP is also helpful in reducing the risk of pregnancy in females taking tetracyclines and oral or topical retinoids, all of which can cause foetal abnormalities.
COCPs give a better effect if taken with topical retinoids and/or antibiotics (topical or oral).
Obviously they are only an option for female patients.
(See section on contraception for further information about the Combined oral contraceptive pill.)
Spironolactone
Spironolcatone is a diuretic (fluid tablet) that has anti-androgen effects and it is very effective in reducing acne. It can cause an increase in serum potassium and this may need to be checked for, depending on the dose prescribed.
D. Treatments that reduce sebum production
Oral isotretinoin
This oral retinoid produces a dramatic improvement in acne in most people and is indicated for those with more severe acne. It is a synthetic derivative of vitamin A (retinol). It acts on all stages of acne development by reducing sebum production by 90%, which in turn reduces blockages and creates an environment which is not conducive to bacterial growth. This in turn reduces inflammation.
The effect depends on the total dose given , as do side effects. A total cumulative dose of 100mg/kg usually gives good results, although doses of 120 to 150mg are often used. This is usually administered as a daily dose of 0.5mg/kg/day for about six to nine months. (This would equate to 30mg per day for a 60kg person.) Smaller doses several times a week are occasionally adequate for relapsing acne.
Sebum secretion and and bacterial counts return to normal after treatment ceases but more severe acne problems do not recur in most cases. (About 40% of patients achieve long term acne suppression, another 40% experience milder acne recurrences that do not require further oral isotretinoin treatment and 20% that need a further course of oral isotretinoin.) Many people continue on other therapy such as the pill or oral antibiotics after ceasing therapy to prevent the small chance of significant relapse, which is more common in people who are under 16 years of age at the commencement of treatment and in females over 25 years of age.
A flare up in acne is quite common in the first few weeks of therapy. This can be a real problem for people with very irritated acne and can be reduced by introducing the dose gradually over the first month or so and by the simultaneous use of antibiotics (but not tetracyclines, which includes doxycycline and minomycin).
It can only be prescribed by a dermatologist ( a specialist skin doctor) and indications for referral include:
- Scarring
- Family history of acne, especially if scarring occurred
- Failure of oral therapy, either the COCP or antibiotic, after 6 months
- Frequent relapse after cessation of oral therapy
- Significant involvement of neck and chest / back
Side effects of oral isotretinoin
The list of side effects is long and perhaps intimidating. However, while most people experience some side effects, in most cases they are mild, not serious and cease within a month of stopping the medication.
Foetal abnormalities
The most serious problem is that fact that it causes foetal abnormalities. There is a 25% risk of abnormalities occurring in a foetus whose mother was taking this medication while pregnant and a 15% miscarriage rate. Patients should only commence therapy after a negative pregnancy test and not become pregnant until at least one month after ceasing therapy. This is a very important issue and any sexually active woman taking this medication must be absolutely sure that she uses adequate contraception. Doctors carefully consider this requirement when deciding whether a patient is suitable oral isotretinoin treatment.
Rare but more serious side effects of oral isotretinoin
-
Depression, suicide: While studies do not show a association, a few patients have developed depression and rare suicides have occurred in patients being treated with oral isotretinoin. Patients need to be screened for depression / suicide symptoms before treatment and patients and parents need to aware of this risk and of the symptoms of depression in adolescents so that they can identify report worrying symptoms as soon as possible. If depression symptoms do occur, they usually resolve quickly once medication is ceased. Most teenagers on oral isotretinin actually experience improved mood as acne improves.
-
Pseudotumor cerebri (also called benign intracranial hypertension): a rare nervous system side effect (See drug interactions below)
-
Premature closing of bone growth plates (epiphyses) has been shown to occur in laboratory animals and for this reason some doctors prefer to wait until growth has ceased before prescribing the medication.
Less severe but common side effects of oral isotretinoin
-
Skin reactions are experienced by most people using the medication. They include:
- Dry cracked lips (cheilitis)
- Dermatitis
- Partial hair loss (reversible) occurs in about 10% of patients
- Sensitivity of the skin to light causing a rash. Sun burn can be a problem with even very bright indoor light, such as that in a dental chair.
- Fragility of the skin which can be a problem when waxing legs to remove unwanted hair (and may cause excess scarring with body piercing).
- Drying out of the mucous membrane lining the inside of the nose can result in nose bleeds.
-
Eyes:
- Dry eyes are common. This can cause problems for those wearing contact lenses. The use of liquid tears is helps overcome this problem. It can very occasionally persist for a period after treatment ceases.
- A degree of night blindness can occur and may be a problem, especially for inexperienced drivers.
-
Liver: Elevated liver function tests occur in about 10% of people. Most return to normal when treatment is ceased. Liver function tests should be performed before medication is started to ensure that pre-existing disease is not present.
-
Muscle aches: These occur in about 15% of people but are usually minor and only a problem to very active people / athletes.
-
Head aches
-
Mild mood changes
-
Elevation of blood triglycerides by about 50% (a type of blood fat)
Drug interactions of oral isotretinoin
Tetracyclines (including doxycycline and minomycin) and oral vitamin A should not be used in conjunction with oral isotretinoin as they increase the risk of the side effect pseudotumor cerebri occurring.
Review needs to occur every six to eight weeks or sooner if problems occur.
Treatments with light and laser
Light
Blue and longer wave light treatments have been shown to reduce acne through reducing bacteria populations. (They do this by stimulating the production of porphyrins in the bacteria and producing other destructive compounds.)
Laser
The use of lasers to cause heating of the skin that selectively injures pilosebaceous glands is also useful in reducing acne. It is used in patients in whom drug treatments have failed or in those who do not wish to use long term medication.